Share:
Suicide: Resilience means getting and giving help
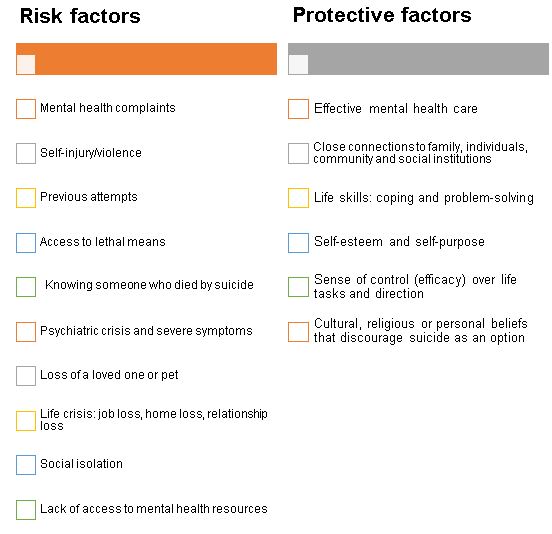
Health care workers are at a higher risk than the general population for mental health struggles and suicide, especially in the COVID-19 pandemic, education changes and the aftermath of our community fire disaster .
This is not a sign of weakness but, rather, repetitive exposure to high stress, trauma and crisis. Unaddressed symptoms such as work pressure, depression, burnout, “survivor guilt,” insomnia, exhaustion and anxiety can increase the risk of suicidal thoughts and actions. Ninety percent of people experiencing a suicidal crisis give some cues or warning to those around them; this is a cry for help.
Warning signs:
- Increased risk-taking such as ignoring orders, refusing PPE, instigating conflict, increased substance use or abuse.
- Comments suggesting a desire to die or not be here.
- Buying a gun or talking about guns and weapons in a heightened way.
- Isolation or withdrawal.
- Deep sadness or hostility.
- Talking about being a burden to others.
- Showing rage or talking about seeking revenge.
No matter what your job role, here’s how to help:
- If you believe someone is considering suicide, no matter their age, you must be willing to directly ask them. “Are you thinking about suicide or wanting to kill yourself?” Asking this can be intimidating, but it is the most effective way to address the person’s deep suffering.
- Offer to assist the person to get help right away. Ask, “Will you go with me to get help?” or “Will you let me assist you to get help?” If you are on the phone with them, try to stay on the line until someone arrives. Ask, “Can we call someone to be with you now?” “What would help you be safe right now?”
- Refer the person (or take them) to a medical or mental health professional. Law enforcement can be called upon for a welfare check. If possible, stay with the person until help arrives.
Here’s how licensed clinicians (RN, LPN, MD, DO, NP, PA, LCSW), can help patients:
- Identify patients at risk for suicide and ask screening questions.
- Assess severity of symptoms using the C-SSRS scale.
- Notify the provider immediately and implement suicide precautions per protocol and suicide precautions policy.
- Create a safety plan and continue to monitor, assess and support safety.
Acknowledging the unprecedented circumstances and the variety of mental and emotional distress symptoms is key. Resilience is enhanced when we get the help needed to recover from overwhelm, mental health challenges and life-threatening suicidality.
Here is an empowering video to help us all confront and help the realness of suicide in our community.
RESOURCES
Asante EAP 24-hour Crisis Line
(866) 750-1327
National Suicide Prevention Lifeline
(800) 273-TALK (8255)
SAMHSA National Helpline
(800) 662 HELP (4357)
SAMHSA Disaster Distress Helpline
(800) 985-5990
Crisis Text Line
Text HOME to 741741
Transgender Lifeline
(877) 565-8860
Jackson County Crisis Line
(541) 774-8201
Jackson County Non-Emergency Sheriff Office
(541) 774-6800
Josephine County Mental Health Crisis Services
(541) 474-5360
Josephine County Non-Emergency Sheriff
(541) 474-5123
If you have a question, please contact the author or relevant department directly.



3 Comments. Leave new
Thank you, Jennifer. Well presented. Timely. Thank you for your care for our staff. Thank you for your care for me.
Important message, thank you.
Thank you, Jennifer! Such important information and a reminder how we all play a part in preventing suicide. Well done!