Share:
Medication history and our collective presence — why we care
“If I have ever made any valuable discoveries, it has been due more to patient attention, than to any other talent.” — Isaac Newton
Medication history is a key part of discovering the clinical narrative about our patients. What they tell or show us about their medications, whether in the form of a list on paper or a bag of pill bottles, helps us understand their past before admission so that we can plan for their best care through discharge.
On hospital admission, more than half of patients have at least one or more unintended medication discrepancies, a critical fact associated with about 33% potential moderate harm and 6% severe harm.1 Every year, the Asante Medication History Committee reports the rates of medication history and reconciliation discrepancies to a national safety organization called Leapfrog, which in recent past has granted ARRMC, ATRMC and AACH positive “report cards.” Starting this year, Leapfrog will publish annual hospital discrepancy rates for the public.
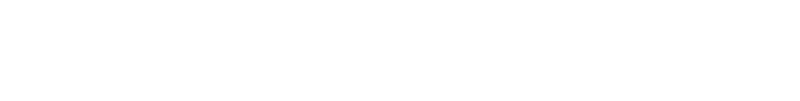
In addition to national reporting, the committee has been gathering specific metrics internally to help visualize our focused areas for improvement. Among the key points being measured are:
- The rates of initial medication list review marked by ED nurses as “in progress” or “done” in EPIC before medication reconciliation.
- The rates of initial medication list review “done” by ED or floor nurses.
Both are currently trending favorably about 81% and 83%, respectively, compared with the goal of 90% across our system.
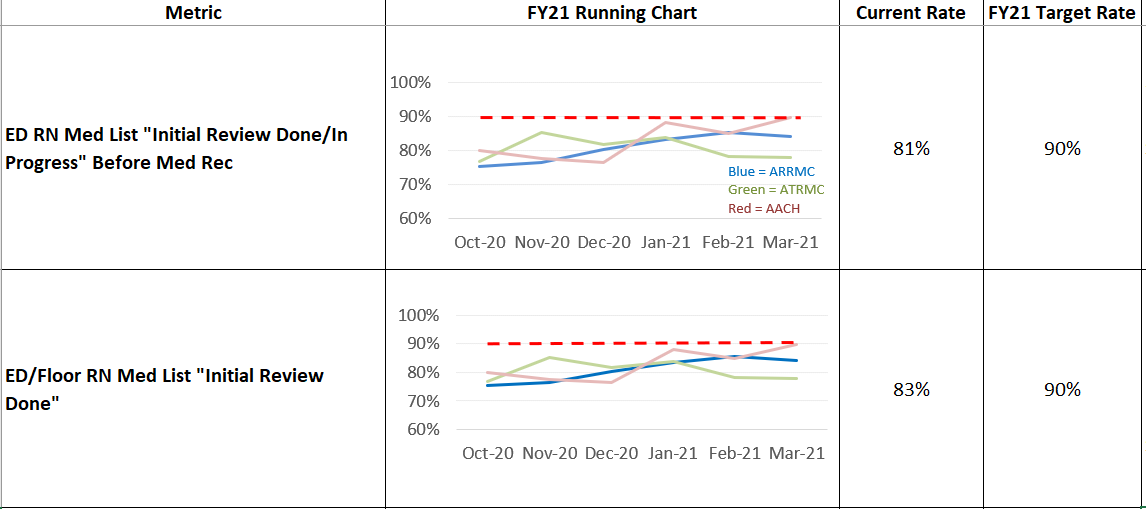
At ARRMC, the rates for these dual measures have significantly improved since last July when Rob Koning, ARRMC ED manager, launched a “medication history track board” in the ED core station to help nurses and providers track in real time the names of patients whose medication lists have yet to be reviewed. Rob’s track board, also emulated by ATRMC ED, is now being considered for use in AACH ED.
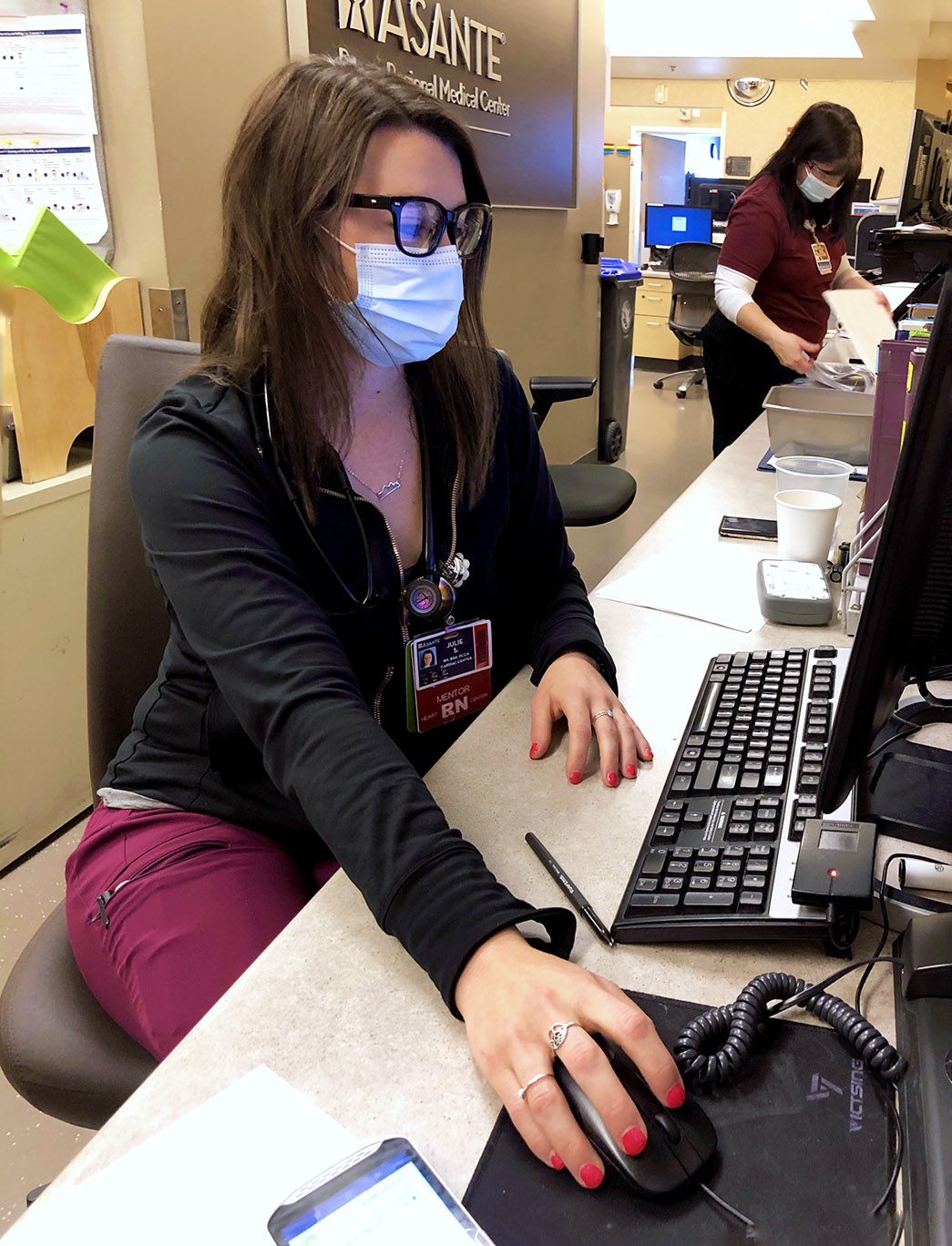
Rob demystifies the recipe for our joint success with ED. “The ED has worked closely with Lexie Karetnick, Epic analyst team lead, to help create a tool that would bring med history completion to the front and center of attention for our nurses who are busy caring for multiple patients,” Rob says. “The ED nursing staff are really owning this initiative and working hard to review initial med list as early as possible in our patients’ stay.”
His commitment to improving the accuracy and timeliness of medication history underscores the tangible goals set of the committee, as expressed by its co-chair, Paisley Meyer.
“As health care professionals we all work to keep our patients safe,” Paisley said. “Ensuring an accurate medication history helps prevent medication errors and polypharmacy, two factors that contribute to adverse outcomes, hospital readmissions and increased cost of care. Part of providing the highest quality care to our patients is ensuring the best possible medication history is recorded for reconciliation at the time of admission. Nurses must work collaboratively with pharmacists and physicians to produce the best medication history possible, each bearing responsibility for the final product.”
Paisley has recently created a practical route for providers to swiftly convey patient-specific feedback about the quality of the medication list reviewed. By pinpointing near-misses and corrections in the medication history and reconciliation process, these reports along with RERs submitted by nurses, pharmacists and other health care teams encourage the committee to continue asking important questions: What might have happened and how could we transform the experiences of our patients toward improved safety and care?
Yet the most pressing question persists in our discoveries: Why should you care about medication history?
Dr. Tim Johnston, one of the committee’s physician champions on the committee, engages us from the spectacular view of a visionary explorer.
“There are many things that can contribute to good health or alter the course for a person when he or she develops an illness,” he said. “In the most extreme situations, surgery or strong medications are needed. Most people are familiar with the surgeon’s tool — the scalpel — but for most other physicians, medications are our scalpel. Understanding what medications our patients have already taken is a vital step in knowing appropriate next steps to help them heal. Without a clear understanding, patients may be in danger from drug interactions, accidental overdoses, duplicate medications or failure to recognize a side effect.
“Treating a patient without an accurate medication history is like reading the middle of a book without knowing the beginning and thus creating an ending that is unplanned and unpredictable. That may be exciting, but I sure wouldn’t want to be the main character.”
If you have a question, please contact the author or relevant department directly.