Share:
How we’re reducing hospital-acquired pressure injuries
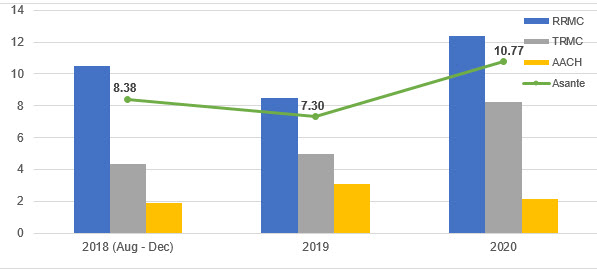
Pressure injuries are a complex problem that can result in long-term and possibly irreversible skin damage, prolonged hospitalization and higher treatment costs. They affect an estimated 1 to 3 million people in the United States every year, with the prevalence of pressure injuries in hospitalized patients estimated to be 5 to 15%, and as high as 49% in the intensive care setting.
Treatment for pressure injuries is lengthy and causes significant financial burden for hospital systems. In the United States, an estimated $11 billion a year is spent on pressure injuries, with up to $70,000 for a single wound.
Fortunately, hospital-acquired pressure injuries are generally preventable. For the past several months, Asante has placed special emphasis on preventing and mitigating patient harm from HAPIs, beginning with a survey to identify the barriers to pressure-injury prevention.
We discovered there were opportunities for improvement in knowledge of interventions recommended for high-risk patients; knowledge of preventive dressings; pressure, friction and shear-reduction strategies (including specialty beds, dressings, heel protectors, and positioning and turning tools and techniques); managing incontinence; and assessing patients’ nutritional needs.
The survey helped guide the development of a new pressure-injury prevention policy and education plan that will be rolled out in the coming months.
The new policy will include a pressure-injury-prevention bundle, an evidence-based, structured approach to improve care processes. When performed collectively and reliably, these bundle elements have been proven to improve patient outcomes and include the following elements:
Standardized risk assessments
- Conduct a comprehensive skin assessment.
- Use the Braden scale to assess risk of developing a pressure injury.
Pressure, friction and shear reduction
- Avoid positioning patients on an area of known injury.
- Reposition high-risk patients off bony prominences such as the coccyx and heels.
- Use pressure-relieving devices (e.g. seat cushion, prevention dressings, heel offloading boots).
- Assess skin beneath medical devices.
- Use an appropriate support surface/bed type.
Positioning and mobilization
- Change position every two hours or more as needed; avoid areas of redness or injury.
- Encourage early mobility using the Asante Mobility Tool.

Moisture reduction and skin care
- Assess pressure points, temperature and skin beneath devices.
- Keep skin clean and at normal moisture.
- Clean skin promptly after episodes of incontinence.
- Use barrier products as indicated.
Nutrition
- Ensure patients receive adequate nutrition.
The initial education plan will help develop foundational knowledge, skills and competencies to identify and prevent pressure injuries. Pressure injury trends and data will continue to be shared monthly at the system-level HAC and patient safety committee meetings to identify opportunities for improvement, including continued education and training focused on reducing pressure injury rates. These efforts require a multidisciplinary approach to prevent hospital-acquired pressure injuries and ensure existing pressure injuries don’t worsen during hospitalization.
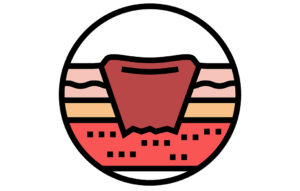 What is a pressure injury?
What is a pressure injury?
A pressure injury is localized damage to the skin and underlying soft tissue, usually over a bony prominence or related to pressure from a medical device. The injury can present as discolored intact skin or an open ulcer and may be painful.
The injury occurs as a result of intense pressure, prolonged pressure or pressure in combination with shear. Patients can come into hospitals with a pressure injury or acquire it during their stay, otherwise known as hospital-acquired pressure injuries, or HAPIs.
If you have a question, please contact the author or relevant department directly.