Share:
How Asante is improving hospital capacity
We all feel the effects of too many patients and what it’s like not having enough beds or staff. Diversions, long wait times and delays in the ED are hospital-wide issues involving more than just ED operations.
Other familiar hospital-wide challenges include a mismatch of bed and staff capacity, demands for specialized clinical services, inefficient processes for transferring and discharging patients.
Achieving hospital-wide patient flow, and ultimately improving the outcomes and experience of the patient, requires an appreciation for the entire system of care — not just the viewpoint from the individual unit in which we typically work.
This lack of inpatient capacity results in delayed or canceled surgical procedures, patients being boarded in other inpatient units (e.g., SSU, PACU or Women’s Services), and boarding in the ED due to lack of inpatient beds.
Meeting the challenges of capacity management is hard, but it is critical work when we think about improving patient care and helping to manage staff workload.
Why does capacity management matter?
Capacity management is key to predicting and planning for current and future needs. By closely monitoring our capacity levels and making the best use of our resources, we can prevent overcrowding and long wait times, which compromise patient safety and affect outcomes.
Capacity management allows us to plan for emergencies and unexpected events such as pandemics, natural disasters or spikes in patient demand. As leaders and clinical staff, we must prioritize capacity management in our daily operations and decision-making to provide our patients the best care.
Asante clinical teams have been charged by Asante to work together with the resources and expertise from across the system to:
- Reduce lengths of stay.
- Improve throughput of patients in the hospital system.
- Develop programs to effectively manage capacity at each of our hospitals.
The Asante Capacity Initiative ensures Asante clinicians and community members are aware of key strategies and can contribute to them. To do this, physician and nursing leaders are working via interdisciplinary input through teams:
The Average Length of Stay, Capacity and Throughput Governance committee
This steering committee is partnering with the Edgility team. Edgility is a capacity management and throughput consultant that provides guidance for efficiency while setting up the infrastructure and platform for the larger vision of the Asante command center.
Key performance indicators are focused on discharge efficiency and velocity with the end goal of increased capacity.
The Estimated Date of Discharge team
The EDD team has been working hard to develop a process for estimated date of discharge, discharge milestones and delays to discharge. The most important part of this workflow is not necessarily captured in the patient record — it is the conversation all care team members have with the patient and their family about discharge, beginning at admission.
Addressing the plan in advance allows for potential delays to be identified and addressed in a timely manner.
The Average Length of Stay rapid action team
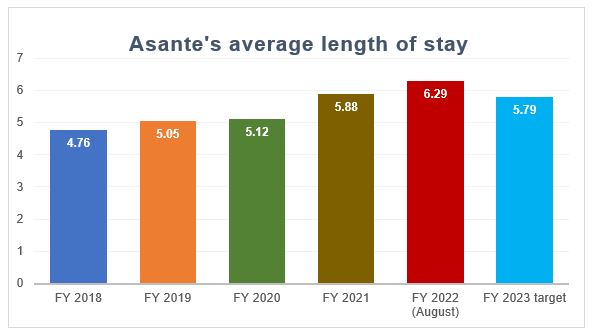
Asante’s average length of stay has steadily increased over the past five years. This year’s length of stay target is 5.79 days — about half a day less than in 2022. For an average 300-bed hospital, reducing ALOS by one day can be the equivalent of 65 new beds.
This team will focus on gathering feedback and enhancing discharge; discharge milestones; identifying and eliminating barriers to discharge; case reviews and state advocacy.
While our current initiatives are focused on process metrics related to estimated date of discharge, throughput and discharge management, these focal points are dynamic and will shift as we optimize our process toward a Transfer Admit Center redesign using Smart Operations. This will provide real-time data management to improve patient information, patient flow and care transitions.
Over the coming months, you will continue to learn about the elements of our capacity management plans. Your feedback is critical to new policies, procedures and workflows. Continued curiosity on how we can reduce discharge barriers, improve communication, innovate new ideas, provide constructive feedback, participate in change, and make today more efficient than yesterday is important as we work to provide quality health care services.
Thank you for your dedication to our patients and for your teamwork!
WORDS THAT WORK
Download for easy reference:
Estimated date of discharge
Transfer between facilities
If you have a question, please contact the author or relevant department directly.