Share:
Patient falls remain a risk
Every year, somewhere between 700,000 to 1 million people in the United States fall in the hospital, causing fractures, lacerations or internal bleeding. Falls not only cause immediate patient harm, they also lead to an increase in health care utilization.
Being hospitalized puts patients at further risk for falls due to illness and the newness of the hospital environment. Unfamiliar surroundings, medications and treatments given in the hospital setting, along with decreased activity, can cause patients to become confused, weak and unsteady. Patients who were active and independent at home may need help to complete simple activities safely while in the hospital, including getting out of bed or using the bathroom.
Research shows that close to one-third of falls can be prevented. Fall prevention involves managing a patient’s underlying fall risk factors (e.g., problems with walking and transfers, medication side effects, confusion, frequent toileting needs) and optimizing the hospital’s physical design and environment.
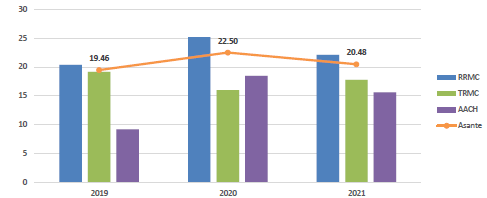
Asante’s fall rates have improved since 2020 but are still higher than 2019. We have more work to do.
The following universal fall precautions should be implemented for all patients receiving care at an Asante hospital (Asante Fall Reduction Program 400-PCS-NURS-0003):![]()
- Familiarize the patient with the environment.
- Keep call light, telephone and all personal items within reach.
- Maintain adequate lighting.
- Use double-treaded socks.
- Remove clutter in the room, keep floor surfaces clean and dry, and clean up spills promptly.
- Follow safe patient handling practices.
- Conduct purposeful rounding as outlined in the patient care bundle.

- Implement delirium prevention strategies.

- Promote early ambulation/mobilization.

- Communicate individual patient fall risk with all members of the health care team.
- Educate patient and family on fall precautions.
Fall interventions also should be tailored based on patient-specific categories of risk and can include the following (not all-inclusive):
- Schedule toileting that is supervised.
- Use a commode at the bedside.
- Use a bed or chair alarm.
- Assess medications that may contribute to delirium, sedation and increased fall risk.
- Assess need for physical or occupational therapy. Contact provider for evaluation.
- Use therapeutic devices including eyeglasses, hearing aids, walkers, canes and gait belts.
- Consider placing the patient in a camera room or using a patient safety attendant.
Preventing patient falls requires diligence from all members of the care team and includes ongoing risk assessments, tailored interventions to mitigate falls, and communication with patients and family upon admission, as risk changes and upon discharge.
Patient or visitor falls should be reported in Midas+, our incident reporting system, to ensure events are reviewed and opportunities for improvement identified. Fall data and trends continue to be reviewed monthly at the system-level health-care-acquired conditions and Patient Safety Council meetings with a focus on reducing fall rates.
If you have a question, please contact the author or relevant department directly.