Share:
Analysis of disaster charting shows pros, cons and risks
Disaster charting was used across the Asante system during the COVID-19 surge to help staff manage high-acuity patients and the higher volumes. Many staff members felt that this was helpful in streamlining their work, while others felt that it hindered their ability to provide safe, high-quality care.
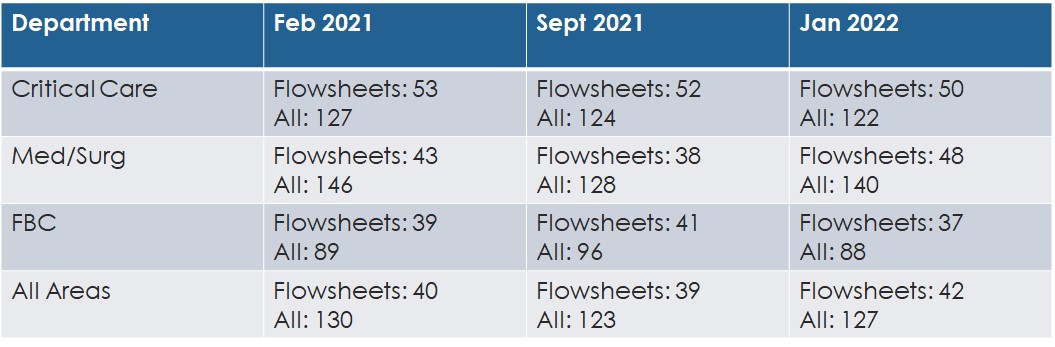
Data was pulled to see how much time was saved for nurses in patients’ charts. The department that saw the largest decrease in time in Epic was our medical surgical department. On average, these departments saved a total of 18 minutes of time in Epic throughout their shift.
While some department areas saw a decrease in time, other departments ended up spending more time in Epic during disaster documentation as shown in the table.
Should we use disaster charting during our current staffing crisis?
Per the policy and best practice, it should be used for short-term disaster events. The staffing crisis is anticipated to be long-term across the nation. Disaster charting could be turned on for specific departments, for short periods of time, if deemed necessary.
Who decides if disaster charting is turned on during a staffing crisis?
Incident Command would make the decision to turn it on.
What are the negative impacts of disaster charting?
- When required documentation was reduced to meet disaster documentation requirements, standards of care were not always met. This impacted the care patients received.
- New staff orienting and travelers lacked the guidance and direction provided by required documentation in Epic.
- Impacts EWIF scores (acuity/intensity not captured accurately).
- Quality and prevention of HAIs/HACs negatively impacted.
- Unable to review documentation that relates to poor outcomes because it did not exist.
- Unable to garner opportunities for improvement because documentation did not exist.
- Increased burden on following shifts and the interdisciplinary team to understand patient’s progress in their plan of care as documentation did not exist to support it.
What are some alternatives being looked at by leadership to alleviate the burden of charting?
- Clinical leadership is working closely with the Epic team to look at functionality that would allow better efficiencies in Epic.
- Turning on disaster charting on for specific departments experiencing staffing issues for short periods of time.
- Working with staff who spend exceedingly more time charting than other staff.
If you have a question, please contact the author or relevant department directly.



1 Comment. Leave new
I’d like to know more about this statement: “When required documentation was reduced to meet disaster documentation requirements, standards of care were not always met. This impacted the care patients received.” Was the lack of additional charting what caused us not to meet standards or care or negatively impact patients’ care, or was it the overall situation (decreased staffing, many travelers, high acuity patients, high census, etc) that led to this? There may be a correlation, but I don’t know that the decreased charting requirements can be labeled as the cause since disaster charting is only implemented when we are in a crisis-type situation.